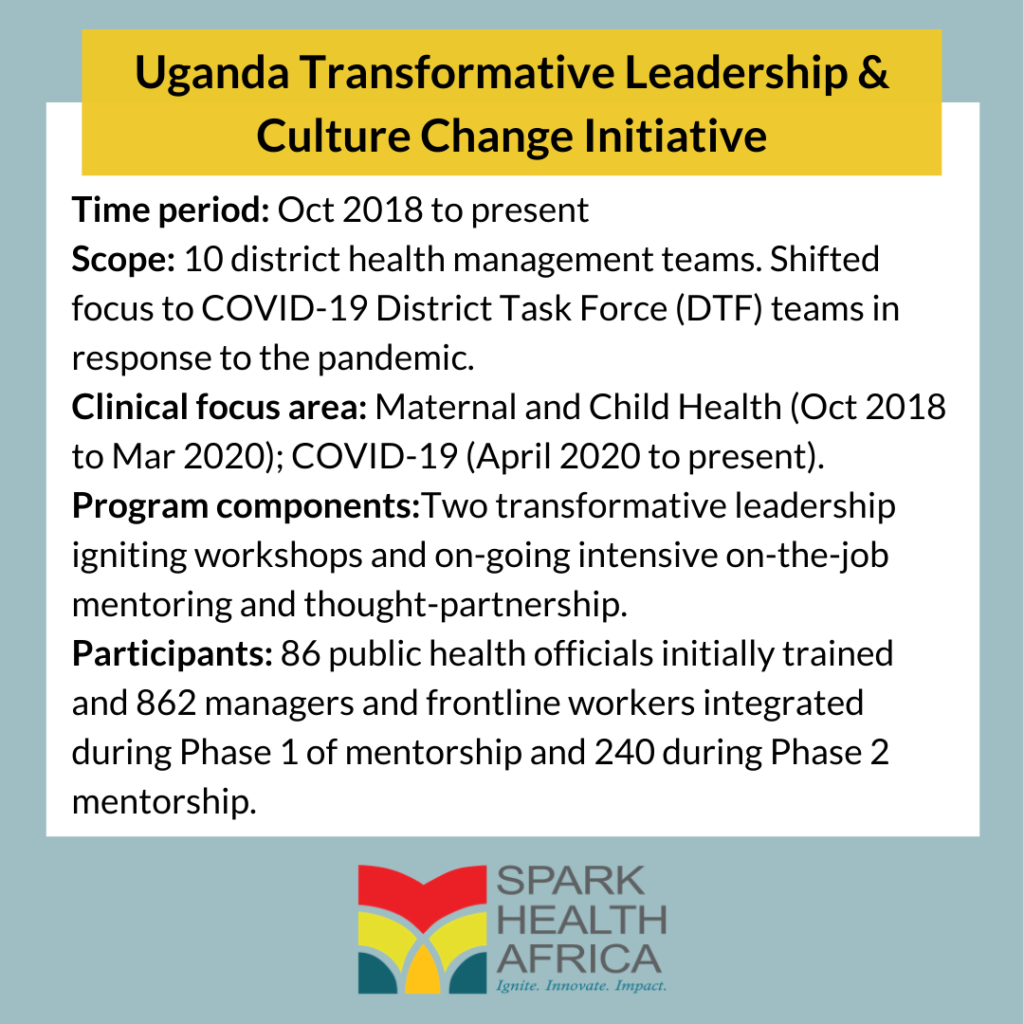
The Ugandan Ministry of Health partnered with Spark Health Africa in 2018 to conduct a transformative leadership and culture change initiative. The transformation journey for district health management teams starts with instructive training on a suite of modules covering management skills and leadership principles. Spark Health Africa then mentors the teams to hone core these skills into competencies (i.e., skills + knowledge + ability).
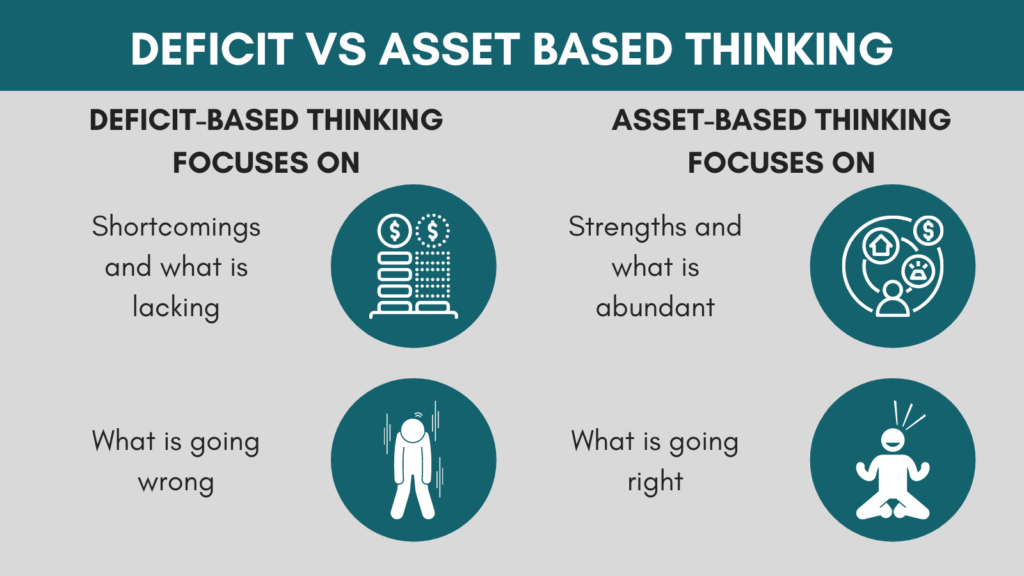
In one of our key modules, Behavioral Finance, we increase awareness and appreciation of asset-based thinking over deficit-based thinking. We also encourage teams to develop strategies that effectively take advantage of existing assets to develop and implement context-specific solutions to address healthcare service delivery challenges.
This article explains why asset-based thinking leads to a more effective workforce than the more common deficit-based approach. We also illustrate asset-based thinking benefits using stories from Ugandan district health management teams.
The status quo: A deficit-mindset
In aid work- the name gives it away- the prevalent way of thinking is based on a deficit mindset – an expectation to receive aid passively, in perpetuity. African governments and their health systems have been recipients of donor funds for decades. This dependency has shifted responsibility away from host governments. Constant funding streams have also created stockpiles of assets that may no longer be efficiently and effectively utilized because beneficiaries expect assets to be replenished.
The reality is that reliance on external funding is unsustainable. What was once a stable inflow has been on the decline for years. Since 2010, donor governments have been reducing aid contributions to Africa. The global economic fall-out from the COVID-19 pandemic has worsened this decrease in aid flows from high-income countries. African countries risk significant disruptions in service delivery and healthcare gains if governments cannot do more with existing resources once the tap fully closes.
Over the past decade, Spark Health Africa has supported district health management teams across Africa to change how they look at and use their assets to solve everyday challenges. We advocate for an asset-based approach to cushion against an over-reliance on donor aid as a sustainable way to tackle healthcare delivery challenges.
What is asset-based thinking, and why is it important?
An asset-based approach is a way of thinking that promotes the identification of protective factors that support communities’ health and well-being. Protective factors include a sense of purpose and a commitment to learning, family and supportive networks, political democracy, and social justice.
Health care service providers that take full advantage of all resources at their disposal to co-create solutions with communities create positive outcomes. Likewise, communities that actively participate in generating demand for healthcare services and holding their service providers accountable for their actions and performance create social accountability.
Insights from Uganda Ministry of Health District Management Teams
Working with select district health management teams in Uganda, we have picked up valuable insights on asset-based thinking over their transformation journey.
1. Reframing the mindset towards assets requires champions to increase asset-based dialogue and showcase the benefits that come with asset-based thinking
Across all districts, the team champion is at the center of the transformative agenda. In some districts (Tororo, Bushenyi, Mbarara, Mityana), the District Health Officer, who is the organizational leader, plants the seed for mindset change and leads the implementation of activities to change the overall work culture. In other districts (Kayunga, Bugiri, Iganga, Mukono), the Chief Administrative Officer, who is the political leader, is the champion that shares their vision for the culture of how assets from the community and municipal system are identified and used. In other districts (Bushenyi, Iganga), champions also emerge from the broader team outside of technical and political leadership.
Deliberately reframing and increasing frequency of conversation around asset-based thinking signalled a shift in work practices. In Iganga District, the district health team would previously autonomously and unilaterally select areas that they visited for community immunization outreach, with poor results. Root cause analysis revealed that the community was unhappy with this indifference and deliberately absconded from these outreach visits. Living in the same communities they served, health workers did not take long to report this to the district health management team. The team reflected on all the vices that propagated this poor practice of mistreating communities and made an about-turn. Before any visit, the district health management team involves the community in deciding where to locate an outreach site to serve everyone, especially marginalized communities. Furthermore, the district health management team leverages village leaders to create demand for immunization services at no additional cost.
A new language emerged among all participating district health management teams. Teams use the term “sparked” to signify and identify with a person or a group that has been transformed from the old way of doing things. It indicates the adoption of a new work ethic that values teamwork and collaboration with the community. Infusion of transformative thinking through a new language, coupled with the showcasing of emerging best practices of how teams are making use of existing physical assets and relationships with private sector partners and communities, has accelerated the diffusion of the work culture change agenda.
2. Having a cleary defined vision allows teams to rally more stakeholders, including the community, behind that vision
In 2019, the Mbarara district struggled to break the 90% annual target coverage for deliveries conducted in a healthcare facility (instead of at home). The first thing the team did was conduct an assessment to review, understand, and map the district’s assets. The process involved going to the health facilities and taking stock of human, physical, and financial assets in the system. The team also reached out to the community and business sector to understand what they could contribute to the assets pool.

After identifying potential assets, the next step was to secure them for deployment. The Mbarara District Health Officer crafted a public-private partnership project proposal that recognized the full arsenal of support at the district’s disposal. The DHO built a relationship with the private sector collaborators by inviting them to visit the dilapidated facilities to see the work required.
Visiting the project area also allowed the Mbarara team to engage with the communities to hear their needs directly. The group felt more urgency and a sense of patient empathy after hearing client needs directly. By bringing together the private sector collaborators and the public health service providers to support their community, the DHO successfully took advantage of previously untapped assets.
A leadership style that is developmental and collaborative bolsters an Asset-based approach to work.
The outcome was a win-win that saw the private sector collaborators get positive publicity for supporting the community. The community also benefited from positive Information and Educational material in the form of a beautiful mural painting decorating the children’s ward.
3. Combining assets and co-creating solutions creates resilient health systems and communities
Bushenyi District health management team made deliberate efforts to empower health facility managers to develop meaningful relationships and engage with the community as key stakeholders. All health facilities strategically directed their community engagement efforts to well-defined, context-specific needs that affect health service delivery. They also viewed communities as a critical asset and part of the solution to address problems.
Facility managers at Buyanja Health Centre II, for example, used formal and informal gatherings at Health Unit Management Committee meetings, churches, burials, and ceremonies to mobilize community resources. They used the resources to build a maternity ward closer to the community, so women have a shorter distance to travel for services. Facility managers at Kabushawo clinic, on the other hand, established community-run gardens to provide for mothers receiving maternal and child health services as a way to avoid reliance on external funding to feed clients.
The culture change initiative also facilitated unprecedented collaboration between political and health leadership in the program districts. In Bugiri District, although the Chief Administrative Officer (CAO) directly supervised the District Health Officer (DHO), before the initiative, there was limited engagement between the parties. During the culture change initiative, the DHO motivated his team to adopt a values-based approach to service delivery i.e. to draw on the highest individual and collective values to guide their conduct. As part of this approach district leadership created stakeholder structures from the district council level down to the villages at community level. This resulted in the Resident District Commissioner, who supervises both the CAO and DHO engaging with the culture change work, something which, would not have happened were it not for the direction taken by the district health management team.

Having close links with the voter base, these political leaders have, on one hand, been using their influence to preach a message of trusting the health system. On the other hand, health management teams have moved away from one-sided “sensitizing” communities, which assumes that only the health service providers are fully aware of the health needs of communities and only they can craft a credible solution. Instead, teams now consult the community about their needs and, by engaging with health teams at community dialogues at every level of the stakeholder structures and through radio talk shows, co-create context-specific solutions. This act of co-creation represents the coming together of equal partners, building on their shared assets and strengths, around a common goal. The result is a better use of each party’s assets and contributions to produce sustainable health outcomes and community well-being.
In Kayunga District, the Deputy Chief Administrative Officer, who leads the Public Service in the district and Administration in the district council, on seeing how health teams, through filling job vacancies internally with existing personnel and targeted redeployment, got more work done with less human resources than the other departments, advocated for replicating the culture change initiative across the entire district council.

How can other district management teams begin to develop an asset-based approach mindset?
Decades of receiving donor funds has had a tremendous impact on health outcomes. It has, however, also reinforced a deficit-based mindset amongst recipients. A fatigued donor community is looking to partner with health teams, civic organizations and communities that are innovative and can demonstrate collective impact- doing more, together, with less.
In the spirit of not putting a good crisis to waste, enlightened health management teams can look differently at the dwindling donor commitments, and instead take advantage of the vast array of resources lying dormant at their disposal. Teams can start by reflecting on how they identify and (re)deploy their human resources, not based on education or skill, but on ability and passion. Having motivated personnel in the right areas creates consistency in service delivery, especially during difficult times.
Teams can also look at the communities they serve through the common lens of empathy and engage with them in a sincere manner so that they too can contribute in the crafting of sustainable, homegrown solutions that improve their well-being and that of their families.
What to read next from Spark Health Africa:
- Building resilience: A transformative leadership and culture change approach to health systems strengthening
- Team-building in Uganda: Transforming Workgroups Through Alignment of Goals and Values
- Government-Centered Health System Strengthening: Lessons from the COVID-19 Pandemic in Africa
- How strong leadership in Eastern Cape improved stock medicine availability
